The Impact

Clinically Translatable Immunometabolic Therapy for Pediatric Low-Grade Glioma
- Funding Date: 2024
- Investigator name[s]: Pavithra Viswanath & John de Groot
- Institution: Univeristy of California, San Francisco
Pediatric low-grade gliomas (pLGGs) are the most common brain tumors in children. Total resection is not always feasible for deep-seated or infiltrative tumors. In such cases, patients may require radiation or chemotherapy, which can lead to neurological and cognitive impairments. Although BRAF or MEK inhibitors have shown efficacy, long-lasting responses are difficult to achieve as tumors often recur or progress despite treatment. Tumor-associated macrophages/microglia (TAMs) are the predominant immune cells in pLGGs. Although the specific characteristics of pLGG TAMs are not fully understood, TAMs in gliomas and other cancers typically exhibit an immunosuppressive phenotype by expressing immune checkpoint ligands such as programmed death-ligand 1 (PD-L1) and secreting cytokines like interleukin-10 (IL-10), which suppress T cell cytotoxicity. In a study using low tumor mutational burden 2341 syngeneic orthotopic tumor-bearing mice, POMHEX (ENO2 inhibitor) treatment reduced the number of immunosuppressive PD-L1+ TAMs and increased CD8+ T cell cytotoxicity. Notably, while POMHEX alone inhibited tumor growth, the combination of POMHEX and immune checkpoint blockade led to tumor regression in the mice. These findings support further investigation into the therapeutic potential of targeting TAM ENO2 in pLGGs.

New Treatment Strategies for Pediatric Glioma
Low-grade glioma in children is commonly treated using surgery when safely possible, with follow-up including observation strategies, as well as the use of chemotherapy and radiation which are associated with declines in quality of life and neuro-cognitive function1-3. Thus, there is an urgent need for new treatments that are cancer specific and that avoid long-term side effects. Antibodies are able to bind very specific molecules on the surface of cells. Cells of the same lineage share cell surface molecules and most cell types are marked by unique cell surface markers. This means that antibodies can be developed that are able to bind one cell type but not any other cell types, rendering antibodies highly useful for the development of treatments against cell-specific diseases including cancer. We propose to use our strengths in applying high-throughput technologies and computational biology to develop new antibody-based treatment modalities for children with a low-grade glioma.
- Funding Date: 2024
- Investigator name[s]: Roel Verhaak
- Institution: Yale University
Dissecting interactions between neurons and pediatric low-grade glioma (PLGG) cells to develop better therapies
Dissecting interactions between neurons and pediatric low-grade glioma (PLGG) cells to develop better therapies. Tumor cells usurp neuronal firing to help drive aggressive tumor behavior. Tumor cells also drive neuronal dysfunction, contributing to seizures and cognitive decline. Studying human pediatric low grade glioma cells and adjacent neurons in their natural habitat, an intact tumor-bearing brain, will enable us to: 1). Understand the complex communication between tumor cells and neurons, and 2) Identify targetable signaling pathways. Critically, the neuronal activity-associated translational landscape (synthesis of proteins from messenger RNA–mRNA) remains unknown in glioma generally, and in PLGG specifically. Translation of mRNA is highly selective (only ~50% of mRNAs are translated) and rapid (milliseconds to minutes) compared to gene expression–synthesis of mRNA from DNA (hours to days), representing that translation is critical for the early adaptation of tumor cells to various stimuli driving tumorigenesis. Thus, we hypothesize that translation control represents a key biological pathway enabling cross talk between pediatric low grade glioma cells and neurons; and that characterizing the translational landscape of PLGG will reveal targetable pathways through which neurons and tumor cells interact, leading to novel improved therapies. We propose to utilize freshly isolated tumor-bearing brain slices from mouse models and primary human PLGG to study interactions between PLGG cells and neurons at baseline, in response to inhibition of neuronal activity, and after anti-tumor treatment. We will use MaxOne Multielectrode Array system to map neuronal activity as normal, increased and decreased activity and type of activity. We will dissect regions within freshly isolated brain slices based on the intensity of neuronal activity (hyperactive, normal, hypoactive) in the setting of baseline tumor-neuron interactions, and perform ribosomal profiling to characterize the translational landscape of each region. We will use this approach to decipher the translational control through which human PLGG cells talk to adjacent neurons in their natural habitat: an intact tumor-bearing brain.
- Funding Date: 2024
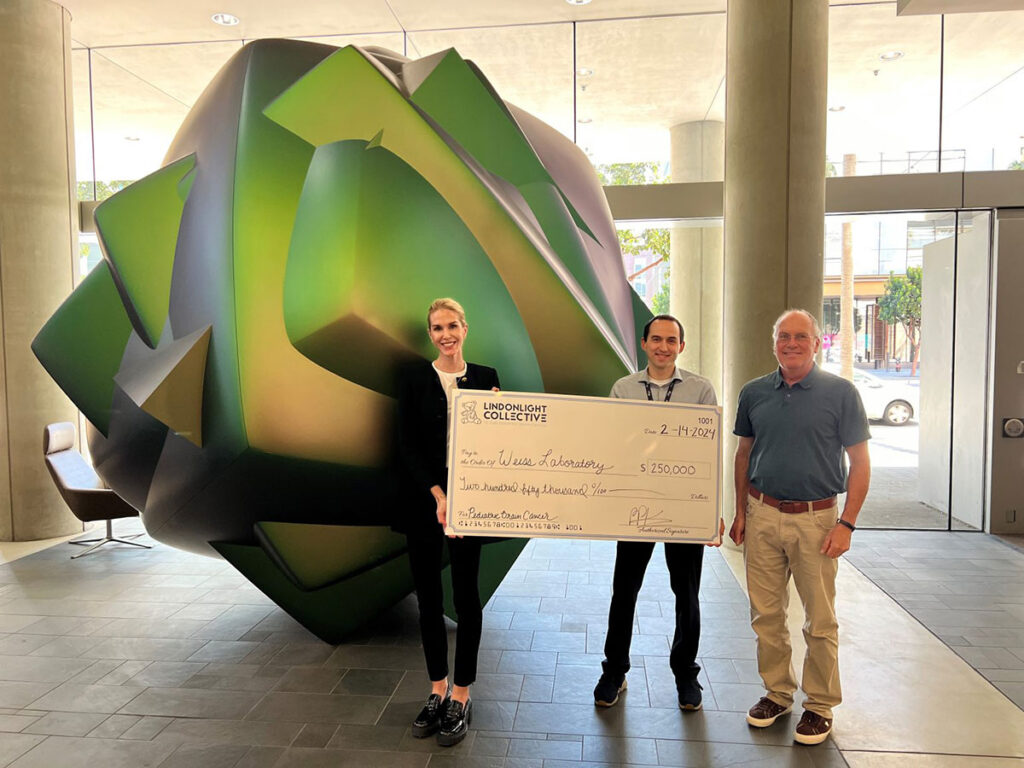
- Investigator name[s]: Ekin Guney and William A. Weiss
- Institution: University of California, San Francisco

CRISPR-based therapy targeting pLGG
The Wilson group proposes use of CRISPR-based genome editing technology to deactivate key driver oncogenes as a treatment strategy for pediatric low-grade glioma (pLGG). Encouraging preliminary observations by the team indicate that the main pLGG driver alterations in the BRAF gene exhibit sequence features that are targetable by CRISPR, which – in the context of low overall mutational burden and limited oncogenic drivers in pLGG – makes CRISPR a compelling treatment option. To address the challenge of brain delivery, the Wilson lab is focusing on an enzyme-centric approach. Ribonucleoprotein (RNP)-based delivery has several inherent advantages: the components can be manufactured at clinic-grade quality, the enzyme is rapidly metabolized, reducing off-target editing and immunogenicity risks, and the CRISPR enzyme’s small size (under 20 nm in diameter) is expected to support efficient diffusion throughout brain tissue. This work represents an important first step towards validating CRISPR as a precision therapy for pLGG.
- Funding Date: 2024
- Investigator name[s]: Ross Wilson
- Institution: University of California, Berkeley

Pre-clinical platform: modelling and characterization of paediatric low-grade gliomas
Numerous studies have emphasized the importance of selecting the appropriate cancer model to successfully translate preclinical research findings into clinical practice. Dr. Hamerlik, who chairs the translational neuro-oncology program at the University of Manchester, will prospectively collect tissue biopsies and create organoid models for pediatric low-grade gliomas with our support. We believe that these models will accelerate drug development, enhance biomarker discovery, and expand research opportunities. Ultimately, this work aims to provide better treatment options and improve outcomes for children with this condition.
- Funding Date: 2024
- Investigator name[s]: Petra Hamerlik
- Institution: The University of Manchester
Therapeutic strategies for FGFR1-driven pediatric low-grade gliomas (pLGGs)
Pediatric low-grade gliomas are the most frequent brain tumor of childhood, and are most frequently characterized by driver events that turn on a pathway called the MAPK pathway. Mutations in a family of genes called ‘FGFR’ represent the second most common way in which the MAPK is turned on in these tumors. The goal of this project is to identify FGFR inhibitors that are able to get to the tumors within the brain and stop the tumors from growing. Our long-term goal is to translate these in clinical trials as therapeutic approaches for children with FGFR-driven pediatric gliomas.
- Funding Date: 2024
- Investigator name[s]: Pratiti (Mimi) Bandopadhay & Rameen Baroukhim
- Institution: Dana Farber Cancer Institute, Inc.

Developing Next-Generation CAR NK Cells for DIPG Treatment
Diffuse intrinsic pontine glioma (DIPG) is a devastating pediatric brain tumor with no effective treatments and extremely poor survival rates. Current therapies offer minimal impact, underscoring the urgent need for innovative approaches. Natural killer (NK) cells are emerging as a promising therapeutic option due to their low toxicity and potential to be used as off-the-shelf therapies, enabling broader access to patients. Dr. Katy Rezvani’s laboratory is spearheading the development of next-generation chimeric antigen receptor (CAR) NK cells designed specifically to target DIPG. The goal of this research is to identify the most effective tumor-specific targets for CAR NK cell engineering. Additionally, the study aims to enhance therapeutic efficacy by arming CAR NK with IL-21 and eliminating inhibitory receptor signaling, further combining CAR NK cells with antibodies such as GD-2, leveraging their ability to improve tumor cell killing. This proposal represents a significant step toward creating safer, more effective, and accessible treatments for DIPG. By advancing CAR NK cell technology and exploring combination strategies, this platform has the potential to transform the therapeutic landscape for DIPG, providing new hope for patients and their families.
- Funding Date: 2024
- Investigator name[s]: Katy Rezvani
- Institution: The University of Texas M.D. Anderson Cancer Center

Antibody-Drug Conjugates (ADCs) for Pediatric Gliomas
Effective drug therapy for low- and high-grade gliomas is a major unmet need in oncology. Antibody-drug conjugates (ADCs) have been developed recently to treat several tumor types. ADCs are designed to consist of an antibody conjugated to a cytotoxic payload. The antibody targets membrane-associated proteins expressed on tumor cells, and the attached payload causes their death. Dr. Pasricha and the UCSF team are focused on the development of ADCs targeting unique proteins that are highly expressed on glioma cells. Engineered, high-affinity antibodies against selected target proteins are chemically linked to suitable payloads. The efficacy and specificity of ADCs are tested initially using in vitro cell cultures models of glioma and human glioma tissue samples, with the most predicted safe and effective ADC(s) to be tested in animal models of glioma. Although the primary focus will be on low-grade pediatric gliomas, the ADC candidates developed in this research are predicted to have efficacy in high-grade glioma as well as some non-glioma tumors outside of the central nervous system.
- Funding Date: 2024
- Investigator name[s]: Neel Pasricha & Alan Verkman
- Institution: University of California, San Francisco

Preclinical Platform: Modelling and Characterization of Pediatric Low-Grade Gliomas
Despite advances on image diagnosis, surgical techniques and biological studies, children diagnosed with low-grade glioma still bear the risk of relapse and potentially poor prognosis. To develop new, effective, and less toxic therapies and to gain better understanding of tumor biology, there is an urgent need of model systems that are clinically relevant and faithfully replicate the biology of childhood low-grade gliomas. Recognizing the inter-tumoral heterogeneity, distinct biological features, and different drug responses, we aim to develop a large panel of novel in vitro and in vivo models for pediatric low-grade gliomas. We will utilize our recently optimized and tumor-location relevant growth culture media to establish 3D organoids, and directly implant patient tumor cells into their matching locations in the brains of immune-deficient mice to create patient-derived orthotopic xenograft (PDOX) mouse models following our optimized surgical procedures. One of the advantages of our model system is that many of the organoids will have their matched PDOX models. The established organoids and PDOX models will be fully characterized to identify all the mutated and dysregulated genes. Since tumor organoids maintained the 3D structures similar to solid tumors and the PDOX tumors are growing in mouse brains that share the maximum similarity to the natural habitat of human low-grade gliomas. This model system should significantly facilitate the understanding of tumor biology and the preclinical test of new therapies. More importantly, all the models will be broadly shared with investigators in the fields to further expediate the studies on pediatric low-grade gliomas.
- Funding Date: 2024
- Investigator name[s]: Xiao-Nan Li
- Institution: Ann & Robert H. Lurie Children's Hospital of Chicago
Pediatric high-grade gliomas are among the most aggressive childhood cancers, with limited treatment options and poor long-term survival. Although immunotherapy offers new hope, single-modality approaches have been limited in their effectiveness. Here, we propose a combination strategy integrating personalized cancer vaccines and endogenous T cell therapy to boost anti-tumor immunity and improve patient outcomes. Personalized cancer vaccines, derived from patient-specific tumor neoantigens, are designed to elicit robust tumor-specific T cell responses. The vaccine stimulates the expansion of tumor-reactive T cells, leading to a strong immune priming effect which can be harnessed by endogenous T cell therapy. Endogenous T cell therapy involves the isolation, expansion, and reinfusion of autologous tumor-reactive T cells to enhance immune surveillance. When combined with a cancer vaccine, pre-existing tumor-reactive T cells are not only comprehensively expanded but also continually reinvigorated, leading to a more sustained and potent anti-tumor response. By implementing this integrated strategy, we aim to enhance tumor-specific immunity in pediatric high-grade gliomas, counteract immune evasion, and promote long-term tumor control. This approach holds the potential to transform the treatment landscape for these devastating malignancies.
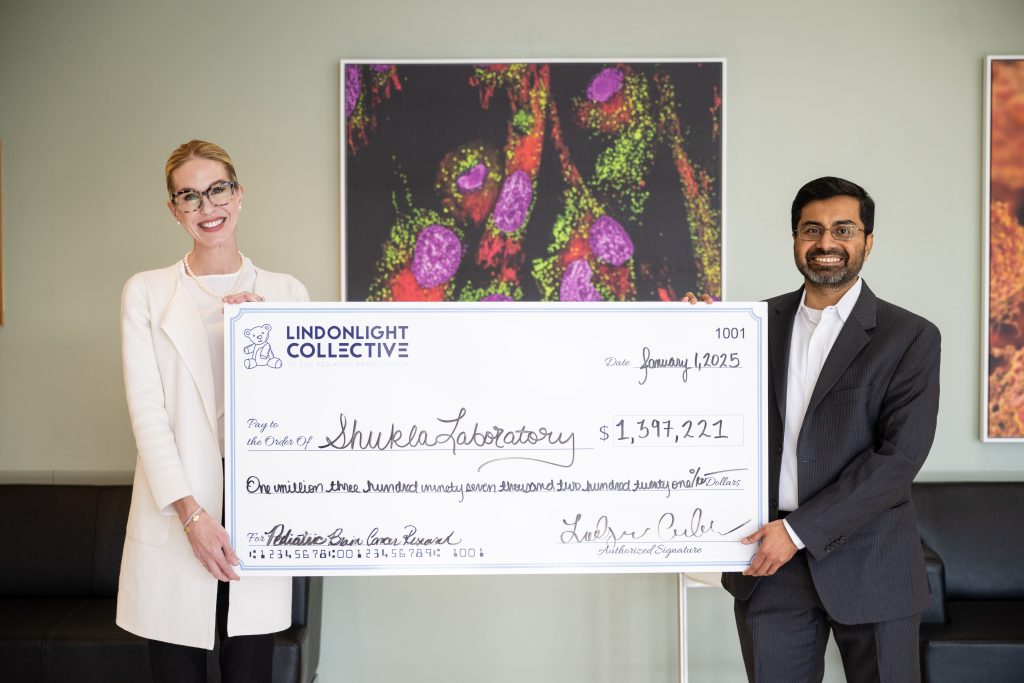
Synergistic Immunotherapy for Durable Tumor Control of Pediatric High-Grade Gliomas
- Funding Date: 2024
- Investigator name[s]: Sachet Shukla
- Institution: The University of Texas M.D. Anderson Cancer Center

This project aims to identify and validate novel immunotherapeutic targets for pediatric and young-adult low-grade gliomas (LGG), the most common brain tumors in children. The team at Children’s Hospital of Philadelphia will combine bioinformatic, proteomic, and immunopeptidomic techniques to uncover surface targets and neoantigens suitable for targeted therapies, such as CAR T-cell therapy and vaccines. The project has two main goals: First, it will use large-scale multiomic datasets from nearly 750 LGG patients to identify potential surface targets. These targets will be validated using several LGG organoid models and patient-derived xenografts with the aim of developing CAR T-cell therapies. Second, the project will predict and validate neoantigens, using a computational method from sequencing data and proteomic assays capable of identifying tumor neoantigens form primary tumor tissue. This data will inform the development of neoantigen-based therapies, such as personalized vaccines. The successful completion of this work will provide new therapeutic avenues for LGG patients and create valuable resources for the broader scientific community, including comprehensive organoid models and data sharing via public platforms.
Combined bioinformatic, proteomic, and immunopeptidomic approaches for immunotherapeutic target identification and validation in pediatric and young-adult low grade glioma
- Funding Date: 2024
- Investigator name[s]: Peter Madsen & Adam Resnick
- Institution: Children's Hospital of Philadelphia

In recent years, chimeric antigen receptor (CAR) T cell therapy has been proven to be curative for children with relapsed leukemias and lymphomas, but this has yet to be realized for pediatric brain tumors. Traditional CAR T cell therapies, however, are limited to targeting proteins that happen to be on the surface of the cancer cell. The problem is that most of the essential proteins that drive tumor progression are inside the cell and thus inaccessible to CAR T cells. However, these intracellular proteins, especially when abnormally expressed as part of the process of a cell becoming malignant, are naturally chopped into small pieces, called peptides, and presented to the body’s immune system by “human leukocyte antigens (HLAs)”, which normally presented pieces of viruses or other foreign invaders of human cells.
The Maris lab has pioneered a strategy to identify tumor-specific peptides recurrently presented on common HLAs and develop “peptide-centric” CAR T cells that can potently kill neuroblastoma, a childhood cancer of the peripheral nervous system, in test tubes and mice. A clinical trial of the first “peptide-centric” CAR T cell therapy for neuroblastoma will be initiated in 2025. Here and in partnership with the Lindonlight Foundation and the Resnick and Madsen labs at the Children’s Hospital of Philadelphia, we will identify pediatric low grade glioma-specific peptides and develop new immunotherapies that will be tested for effectiveness in killing pediatric low grade glioma and likely other types of pediatric brain cancers as a precursor for a clinical trial of our novel immunotherapies.
Peptide-Centric CAR T Cell Therapy: Targeting Intracellular Oncoproteins in Pediatric Low-Grade Gliomas
- Funding Date: 2024
- Investigator name[s]: John Maris
- Institution: Children's Hospital of Philadelphia

This project aims to uncover the distinct biological characteristics of pediatric low-grade gliomas (pLGG), which are rare yet the leading cause of cancer death in children. Previous research has highlighted altered molecular profiles in pCNS tumors, but in part due to the complexity of the tumor microenvironment there remains a gap in identified therapeutic targets. Our project will address this gap utilizing leading-edge techniques, including spatial transcriptomics and genome-scale DNA methylation analysis. We aim to identify specific gene expression and epigenetic changes in pLGG tumors and their potential relation with surrounding cells in the tumor microenvironment. By integrating multi-omic data, we will investigate how epigenetic modifications impact cellular behavior and contribute to treatment resistance in pLGG. Our multi-faceted approach not only enhances our understanding of pLGG biology but also aims to identify high-value therapeutic targets for future clinical trials. Ultimately, the goal is to improve treatment strategies for pCNS patients.
Integrative multi-omics discovery and validation of novel targets in pediatric low grade gliomas
- Funding Date: 2024
- Investigator name[s]: Brock Christensen
- Institution: Dartmouth College

pLGG is driven by KIAA1549-BRAF fusion oncoproteins. Small molecule drugs such as BRAF inhibitors have traditionally been designed to block enzymatic functions of proteins, thus globally inhibiting activity, however, in pLGG patients, global BRAF blockade poses unacceptable toxicity. Recently a new type of drug, known as molecular glues, has been discovered. Molecular glues can remodel protein complexation states to stabilize existing complexes or even bring new proteins together. Approved drugs such as trametinib and avutometinib have shown that molecular glues can prove highly successful in the clinic. These non-degrader molecular glues bind allosterically to MEK and recruit it into non-functional complexes with ARAF, BRAF, and CRAF that more effectively block signaling compared to conventional allosteric MEK inhibitors. Development of MEK:RAF targeting molecular glues represent an attractive alternative approach to inhibitors for targeting KIAA1549-BRAF fusion oncoproteins selectively, by enabling differential recruitment of BRAF WT vs KIAA1549-BRAF via fine-tuning of non-ATP site interactions. Our hypothesis is that selective MEK:KIAA1549-BRAF molecular glues would have a higher therapeutic index than tovorafenib, by reducing the on-target toxicity associated with WT BRAF inhibition. In this proposal, we seek progress towards this goal by building the proteomic and biosensor platforms required, and complementary small molecule libraries.
Targeting KIAA1549-BRAF fusion proteins with molecular glues
- Funding Date: 2024
- Investigator name[s]: Fleur Ferguson
- Institution: Univeristy of California, San Diego

MRI is an invaluable tool for the non-invasive diagnosis and monitoring of lesions in the brain, but despite significant technological progress, a biopsy is still required to confirm a specific cancer diagnosis. Indeed, many lesions observed by MRI are discovered as incidental findings “Incidentalomas”, whose pathological significance (and whether these are actually cancerous) remains difficult to ascertain with current MRI protocols.
The applicant is proposing to utilize a novel algorithm, Diffusion basis spectrum imaging (DBSI), to improve the non-invasive diagnosis and monitoring of these incidentalomas, and specifically distinguish those that represent true pediatric low grade gliomas. The applicants propose to perform systematic DBSI measurements of a large collection of both in vivo and ex-vivo pediatric low grade glioma specimens, and utilize machine learning methods to train the algorithm to recognize specific histological features diagnostic of pediatric low grade glioma. Furthermore, the applicants propose to evaluate DBSI for predicting treatment responses in pediatric low grade glioma, in particular those with worse outcomes such as those in the thalamus and pons. Finally, the applicants will apply their DBSI algorithm to the non-invasive diagnosis of incidentalomas suspected to be pediatric low grade gliomas.
Overall, the successful outcome of the project will result in greater non-invasive diagnostic accuracy of pediatric low grade gliomas, reducing the need for invasive procedures and reduce associated adverse complications.
science.
Improving Non-Invasive Diagnosis and Treatment Monitoring in Pediatric Low-Grade Gliomas Using Machine Learning-based Diffusion Basis Spectrum Imaging
- Funding Date: 2024
- Investigator name[s]: Albert Isaacs
- Institution: The Research Institute at Nationwide Children's Hospital

Pediatric gliomas account for 30% of brain tumors and 10% of childhood cancers, with epidermal growth factor receptor (EGFR) alterations playing a key role. While EGFR gene mutations are present in a subset of gliomas, its protein is overexpressed in over 90% of high-grade gliomas (HGGs), particularly in bi-thalamic diffuse midline glioma and certain H3-wildtype pHGG subtypes. However, no FDA-approved EGFR inhibitors effectively penetrate the brain to target pediatric gliomas. ERAS-801, a novel and selective EGFR tyrosine kinase inhibitor (TKI) designed specifically for malignant glioma, demonstrates superior brain penetration (>350% brain-to-plasma ratio) compared to previous TKIs like Tagrisso. Preclinical studies show that ERAS-801 significantly halts tumor growth and extends survival in pediatric glioma models. This study seeks to further evaluate the ability of ERAS-801 to modulate EGFR signaling, inhibit tumor progression, and explore potential combination strategies in pediatric HGG models. If successful, this research could facilitate the rapid clinical translation of ERAS-801 as a promising treatment option for children with high-grade gliomas.
Targeting EGFR in pediatric glioma
- Funding Date: 2024
- Investigator name[s]: David Nathanson
- Institution: University of California, Los Angeles

Current standard of care results in serious long-term, treatment-related morbidities in 60-80% of pediatric low-grade glioma (pLGG) survivors. Thus, new treatments are needed that not only eliminate disease but also minimize long-term side effects and preserve quality of life. Immunotherapies that can target and eliminate tumors with cellular precision are a promising treatment modality, yet barriers to effective treatment still exist. Tumor cell heterogeneity, limited known tumor-associated antigens, and the ability of tumors to evade immune recognition through upregulation of immune checkpoints represent significant hurdles that must be overcome. To meet this need, we propose a novel “antigen assimilating” multispecific T cell engager (MTE) that will direct immune mediated clearance of pLGG. We hypothesize that an MTE with glioma-selective targeting and optimized immune engagement will overcome the identified barriers to effective treatment and direct a patient’s immune system to eliminate disease while minimizing long-term side effects. It is the overarching goal of this proposal to translate our promising preliminary results into an effective immunotherapy for the treatment of pLGG.
Antigen-assimilating multispecific antibodies for the treatment of pediatric glioma
- Funding Date: 2024
- Investigator name[s]: Jim Olson and Jason Price
- Institution: Seattle Children's Research Institute

Pediatric low-grade glioma (pLGG) is the most common CNS tumor accounting for 30%-40% of all CNS tumors in children. Advances in the understanding of molecular pathways in pLGG have led to the emergence of the mitogen-activated protein kinase (MAPK) pathway as a key driver of pLGG tumorigenesis. While most MAPK oncogenic alterations are observed in the BRAF gene, around 6% of pLGG patients harbor alterations in the fibroblast growth factor (FGF) receptor tyrosine kinase family, a key initiator of the RAS/RAF/MAPK pathway. Specifically, the N546K and K656E mutations within the kinase domain of FGFR1 have emerged as common oncogenic driver mutations. These mutations, which are not typically found in adult tumors, are associated with a poorer prognosis compared to the more common pLGG KIAA1549-BRAF fusion. The goal of this proposal is to initiate the discovery and development of first-in-class FGFR1 N546 and K656 mutant-selective kinase inhibitors for the treatment of pLGG. If the development of such mutant specific inhibitors becomes difficult, we will consider the development of brain-penetrant pan-FGFR inhibitors that are specifically geared against pLGG.
Development of N546K, K656E mutant FGFR small molecule inhibitors
- Funding Date: 2024
- Investigator name[s]: Matthew Hall
- Institution: National Center for Advancing Translational Sciences (NCATS)

30% of all pediatric CNS tumors are pediatric low-grade glioma (pLGG), making it the most common type of brain tumor in children. Recent advances in molecular diagnostics have revealed that the Ras/MAPK pathway is activated in almost all pLGG. The most common driver mutations that activate this pathway occur in the serine/threonine-protein kinase BRAF; the KIAA1549-BRAF (16:9) fusion and the BRAF V600E mutation account for 68% and 62% of all pLGG gene rearrangement and SNV driver mutations, respectively. While multiple drugs that inhibit BRAF V600E have been FDA-approved for the treatment of melanoma and other cancers, none were specifically developed for CNS cancers. This makes a compelling argument for the development of small molecule inhibitors that target the BRAF gene for pLGG. The overarching goal of this proposal is to discover and develop first-in-class inhibitors that specifically inhibit the KIAA1549-BRAF fusion protein. We will also seek to develop brain penetrant pan-BRAF inhibitors for pLGG that target fusion BRAF proteins, the V600E mutant and the BRAF homo- and heterodimers that cause paradoxical activation of BRAF when treated with V600E inhibitors.
Development of KIAA1549-BRAF fusion inhibitors and brain penetrant pan BRAF inhibitors of pLGG
- Funding Date: 2024
- Investigator name[s]: Samarjit Patnaik
- Institution: National Center for Advancing Translational Sciences (NCATS)
Decades of cancer research have focused on the canonical set of protein-coding genes as the central actors of disease biology. Through these investigations, a whole panoply of discoveries and therapeutic targets have been pursued. However, recent work suggests that researchers have been paying attention to only part of the picture. Today, scientists now know that the genome has an additional set of thousands of alternative sites that may also make proteins. Solving these may lead to new insights on disease biology and novel treatments. In this proposal, Dr. Prensner will open this door for pediatric low grade glioma. He will systematically pursue the uncharted “dark proteome”, i.e. the thousands of potential proteins that remain uncharacterized in pediatric low grade glioma. He will use patient samples and disease models to map these entities and explore their therapeutic promise. He will particularly focus on the ability for the dark proteome to activate the immune system through the production of disease antigens. This work may pave a new path towards immunotherapy targets for pediatric low grade glioma
The dark proteome of pediatric low grade glioma
- Funding Date: 2024
- Investigator name[s]: John Prensner
- Institution: University of Michigan

There is a significant unmet need for new therapies to treat pediatric low-grade glioma (pLGG), the most common central nervous system tumors in children and adolescents. Currently there are limited cell lines available for modeling pLGG, which is a barrier for drug development to treat pLGG. We propose here to generate five isogenic pairs of iPSC lines with mutant FGFRs (FGFR1-N546K, FGFR1-K656E, FGFR1-K656D, FGFR3-N540K, and FGFR3-G380R) that are relatively common in pLGG. We will differentiate these isogenic iPSC lines to astrocytes and scale up production for high throughput screening (HTS). We will develop a cell-based FGFR assay measuring the intracellular calcium response after FGFR activation for HTS. We will perform repurposing screens to identify specific inhibitors of the mutant FGFRs for drug development to treat pLGG. We will also apply a matrix-based drug combination screen to identify synergistic drug combination pairs for drug combination therapy that can enhance therapeutic effects and reduce individual drug concentrations to decrease side effects. The cell lines generated will be a useful resource for the community and this platform of a cell-based kinase assay and drug repurposing screen can be used for other low occurrence mutations for personalized medicine development for pLGG.
High-throughput drug repurposing screens of FGFR inhibitors using astrocytes derived from a panel of isogenic human iPSCs carrying pLGG-related mutant FGFRs
- Funding Date: 2024
- Investigator name[s]: Hongjun Song
- Institution: University of Pennslyvania

Brain tumours such as glioblastomas (GBM) and especially pediatric low-grade gliomas (pLGG) are regarded as poorly immunogenic and “cold” tumours. Now, recent data support the view that the pLGG tumour microenvironment (TME) can harbour immune infiltrates that could be (re-)activated. In light of the comparably low mutational burden of pLGGs, only additional neo-antigen release may foster an effective anti-tumour response when combined with immunotherapy. Interleukin (IL)-12 is a master regulator of type 1 immunity with high efficacy in many preclinical tumour models. Unfortunately, IL-12 – even when administered locally – leaks rapidly from the TME and is poorly tolerated systemically, which has hampered clinical translation until today. To address this shortcoming, the vom Berg lab has developed a brain compartment-locked (C-Locked) IL-12 variant characterised by enhanced brain retention and reduced blood exposure. Local therapy with C-Locked IL-12 is efficacious as monotherapy as well as in combination with chemo and radiotherapy in preclinical models of GBM – without peripheral toxicity. Now, they propose to test the combination of C-locked IL-12 with chemotherapies for pLGG, such as lomustine and vinblastine, as a means to trigger antigen release. Planned studies will employ state-of-the-art immunologic tools and preclinical rodent models of pLGG.
Evaluation of Compartment-Locked IL-12Fc as local adjuvant for treatment of pediatric low-grade gliomas
- Funding Date: 2024
- Investigator name[s]: Johannes vom Berg
- Institution: University of Zurich, Switzerland
Children with low grade gliomas may experience substantially different journeys with their disease. Some children have tumors that are easily removed by surgery and never return. Other children have tumors that cannot be safely removed by surgery and their disease spreads throughout their brain and spine. The underlying genetic changes that cause the glioma can be used to predict what the tumor’s behavior. But without surgical intervention, it has not been possible to determine the molecular make-up of a glioma. In this proposal, Dr. Prensner will develop a non-invasive test that aims to deconvolute the tumor’s genetics when surgery cannot be performed. He will use innovative adaptions of gene sequencing and optimize ultra-sensitive diagnostic tools to search for low grade glioma RNA in patient blood samples. By doing so, he hopes to create the first blood test for the diagnosis and monitoring of pediatric low grade gliomas.
RNA liquid biopsy for the non-invasive monitoring of low-grade gliomas on tumor-associated macrophages as therapeutic targets
- Funding Date: 2024
- Investigator name[s]: John Prensner
- Institution: University of Michigan

Antibody-drug conjugates (ADC) represent an important new class of therapeutic that combines the exquisite specificity of antibodies with the potent killing ability of a small molecule payload. While many patients with non-CNS tumors have benefited immensely from ADCs, children with brain tumours have been much less responsive, and pediatric gliomas (PGs) remain the leading cause of cancer-related deaths in children. Recent studies from our labs and others have revealed CD276 protein as a promising target highly overexpressed in virtually all forms of adult and pediatric brain tumors regardless of stage and subtype. While such highly tumor-selective expression of CD276 protein creates an exciting opportunity for antibody-based treatment of PG, currently the successful deployment of effective CD276 ADCs is limited by off-target toxicity caused by the hydrophobic drug payload, a problem shared by ADCs across the field. In this proposal we aim to reduce toxicity by eliminating ADC surface hydrophobicity and successfully treat PG models in vivo. This proposal aims to develop novel ADCs specifically designed to address the unique challenges of PG, with the goal of enhancing treatment efficacy and tolerability.
Development of well tolerated antibody-based therapies to eradicate pediatric gliomas
- Funding Date: 2024
- Investigator name[s]: Martin Schnermann
- Institution: National Cancer Institute, Center for Cancer Research
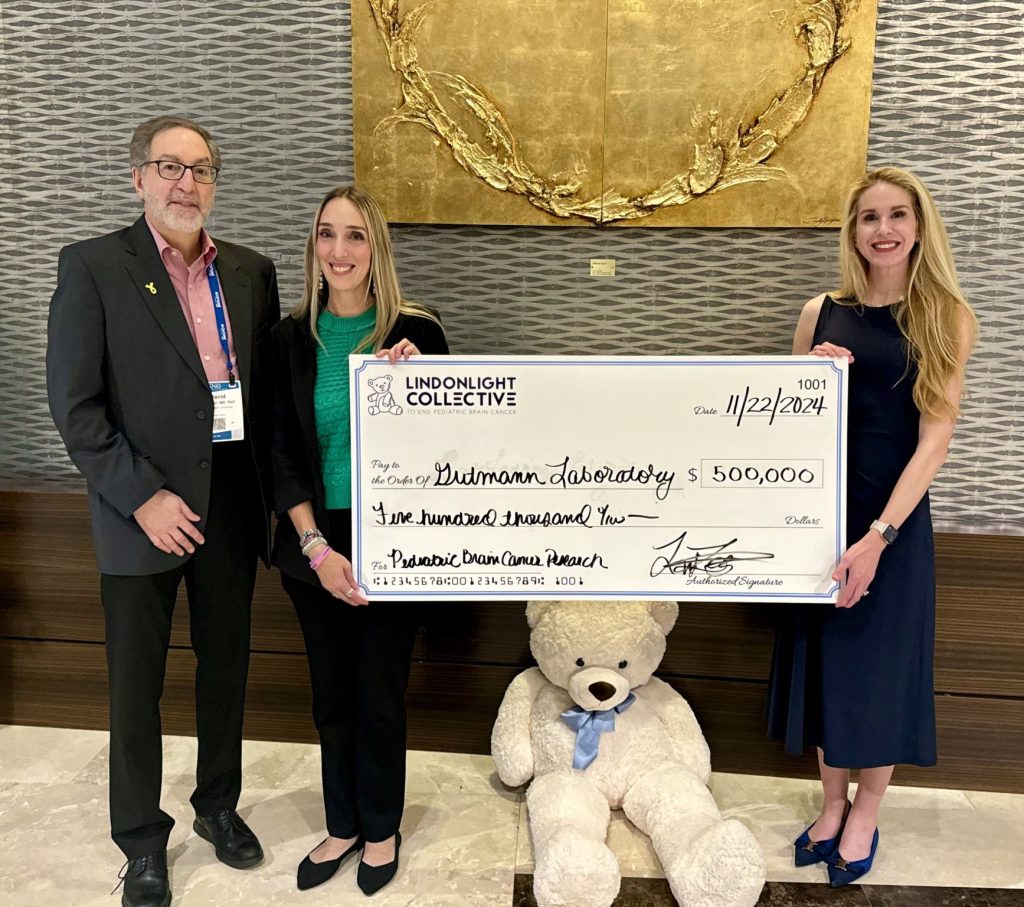
Prior studies from the Gutmann Laboratory have demonstrated that pediatric low-grade glioma (pLGG) growth requires support from immune-like cells within the tumor microenvironment (TME), notably tumor-associated monocytes (TAMs). Unfortunately, currently available in vivo preclinical models of human pLGG growth require that patient-derived pLGG xenograft (pLGG-PDX) tumors be implanted into mice with an impaired immune system and an incomplete TME. To identify and evaluate TAM-targeted therapies, we leveraged RNA sequencing to discover that genetic depletion of Cxcl10 was sufficient to enable pLGG-PDX tumor growth in vivo. The resulting pLGG-PDXs grow for at least six months in Cxcl10-deficient mice and exhibit robust TAM infiltration. Using these novel genetically engineered mice (GEM) as immunocompetent hosts for pLGG-PDX tumors, the overall goal of Drs. Gutmann’s and Anastasaki’s project is to (1) characterize the TAM composition of pLGG-PDX tumors and (2) determine the preclinical therapeutic efficacy of TAM-targeted immunotherapies.
Optimizing humanized preclinical low-grade glioma mouse models for immunologic targeting
- Funding Date: 2025
- Investigator name[s]: David H. Gutmann and Corina Anastasaki
- Institution: Washington University

